CATEGORIES
- Absorbable-Gelatin Sponge
- MR patient monitor
- MRI wheelchairs
- MRI compatible stretcher
- New MRI prodcuts in 2024
- MRI trolleys
- MRI Anaesthetic Machine
- MRI RESPIRATORY
- MRI IV Stand
- MRI compatible stool
- MRI fire extinguisher
- MR transfer board
- MR injector
- MRI finger Oximeter
- MRI Positioning sponge
- MRI anesthesia machine
- Hand Held MR Metal Detector
- MRI coil
- MRI infusion pump
- Pool access wheelchair
- Radiation protection products
- Hospital Furniture
LATEST NEWS
- Why Your Hospital Needs an MR Compatib
- Why Hospital Needs Non-Magnetic Transp
- Why hospitals need MR-Compatible Anest
- Why Ferromangetic detectors are so imp
- Why Hospitals Must Invest in MRI-Compa
- Non-Magnetic Wheelchairs vs. Standard
CONTACT US
- ADD: FLAT/RM A17,9/F SILVERCORP INT'L TOWER 707+713 NATHAN RD MONGKOK KLN HONG KONG
- TEL: +86-13737941709
- FAX: +86-771-6759549
- E-mail: Sarah@hhao-tech.com
FEATURED PRODUCTS
-
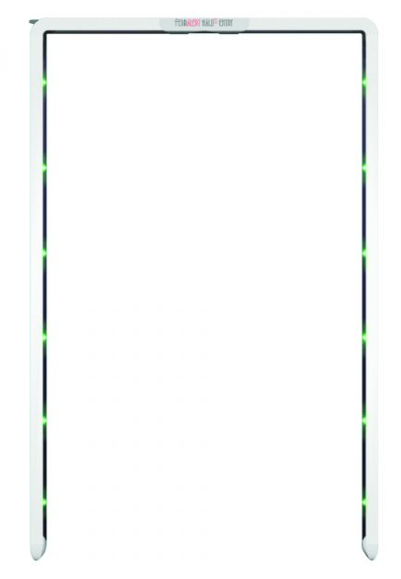
FERROMAGNETIC MRI GATE D
FERROMAGNETIC MRI GATE DETECTOR...
-

MRI Anaesthetic Machine
MRI Anaesthetic Machine...
-

MR compatible patient mo
MR compatible patient monitor...
-
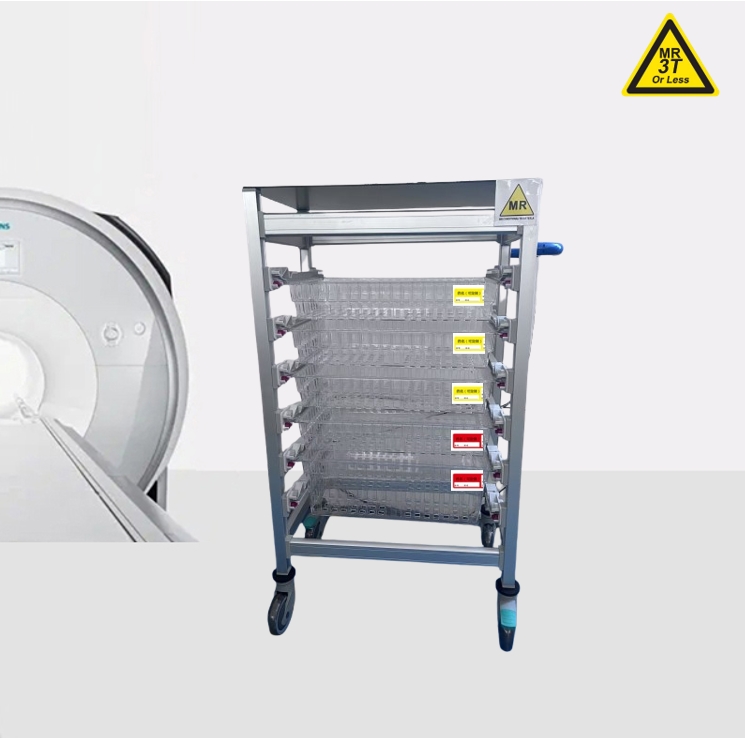
Non-magnetic MRI trolley
Non-magnetic MRI trolley for 5 pcs baskets for 1.5T and 3.0T...
-

MR compatible stainless
MR compatible stainless steel trolley with 2 shelves and 4 dra...
-

MR compatible oxygen cyl
MR compatible oxygen cylinder with 40L capacity...
-

MRI compatible stool for
MRI compatible stool for MR room use...
-

Hydraulic MR stretcher t
Hydraulic MR stretcher trolley/ height adjustable...
-

MRI EMERGENCY CART
MRI EMERGENCY CART, MR compatible emergency cart/ MR compatibl...
-

Nonmagnetic MRI wheelcha
Nonmagnetic MRI wheelchair for 1.5T and 3.0 TESLA...
-

MRI Compatible Anesthesi
MRI Compatible Anesthesia Cart with Accessory Package, Five Dr...
-

Hydraulic height adjusta
Hydraulic height adjustable MR stretcher trolley...

 Sarah
Sarah Sarah
Sarah